“Quality, Safety and Value: The role of Surgical Instruments”

The Association of British Health Industries’ surgical instruments working group consists of over 20 companies who have contributed collaboratively to create this document to share expertise and provide insight into considerations relevant to surgical instruments purchasing.
EXECUTIVE SUMMARY
Surgical instruments are essential for the delivery of modern healthcare. Their use is so widespread that they are easily taken for granted.
The supplier base for instruments is diverse, including small, family owned businesses,and large multinational corporations. What they have in common are complexmanufacturing processes, global supply chains, broad product ranges to suit varying clinical needs and product development with the capacity to innovate as required.
This paper details the role of surgical instruments and how they bring value to the NHS. It highlights the vast range and number of instruments that are needed in the NHS at any one time and,. to ensure that these instruments continue to be safe and fit for purpose, makes the following recommendations:
1. Investment in the replacement of aged surgical instrument inventory should be considered as a priority for NHS spending.
2. The procurement of surgical instruments should be based on overall quality and value, with the demonstration of strong ethical and resilient supply chains recognised and rewarded in purchasing decisions.
3. There should be a focused, sustained and appropriately accredited programme of education into the management and maintenance of surgical instruments. Such a programme could be delivered in conjunction with industry

THE ABHI SURGICAL INSTRUMENTS GROUP
The ABHI Surgical Instruments Group (SIG) is made up of around 20 companies, representing both single-use and reusable devices and supporting products. It sits within the Association of British HealthTech Industries (ABHI), the UKʼs leading HealthTech Trade Association.
The SIG meets regularly to discuss current industry challenges and solutions, and is intended to be a proactive resource for stakeholders. A conduit to the industry, the SIG is committed to continuous improvement within the sector and maintaining a responsible and ethical approach.
The SIG exists to:
- Provide a forum to maintain a responsible and ethical approach, overcome challenges and develop best practice in the supply and use of surgical instruments.
- Educate stakeholders as regards value, quality and condition of surgical instruments and the impact they have on patient safety
- Work alongside procurement professionals to ensure that purchasing frameworks are both sustainable and ethical
- Raise the profile and professionalism of the sector.
- Develop a sustainable marketplace for both single-use and reusable instruments
THE SURGICAL INSTRUMENTS SECTOR
The importance of high-quality reusable and single-use surgical instruments has never been greater to the HealthTech Sector. With the well-publicised NHS budget constraints1, an ageing population, over 10 million operations2 performed each year in England, in just over 3,200 operating theatres3, this clearly creates significant pressure to keep instruments available and fit for use.
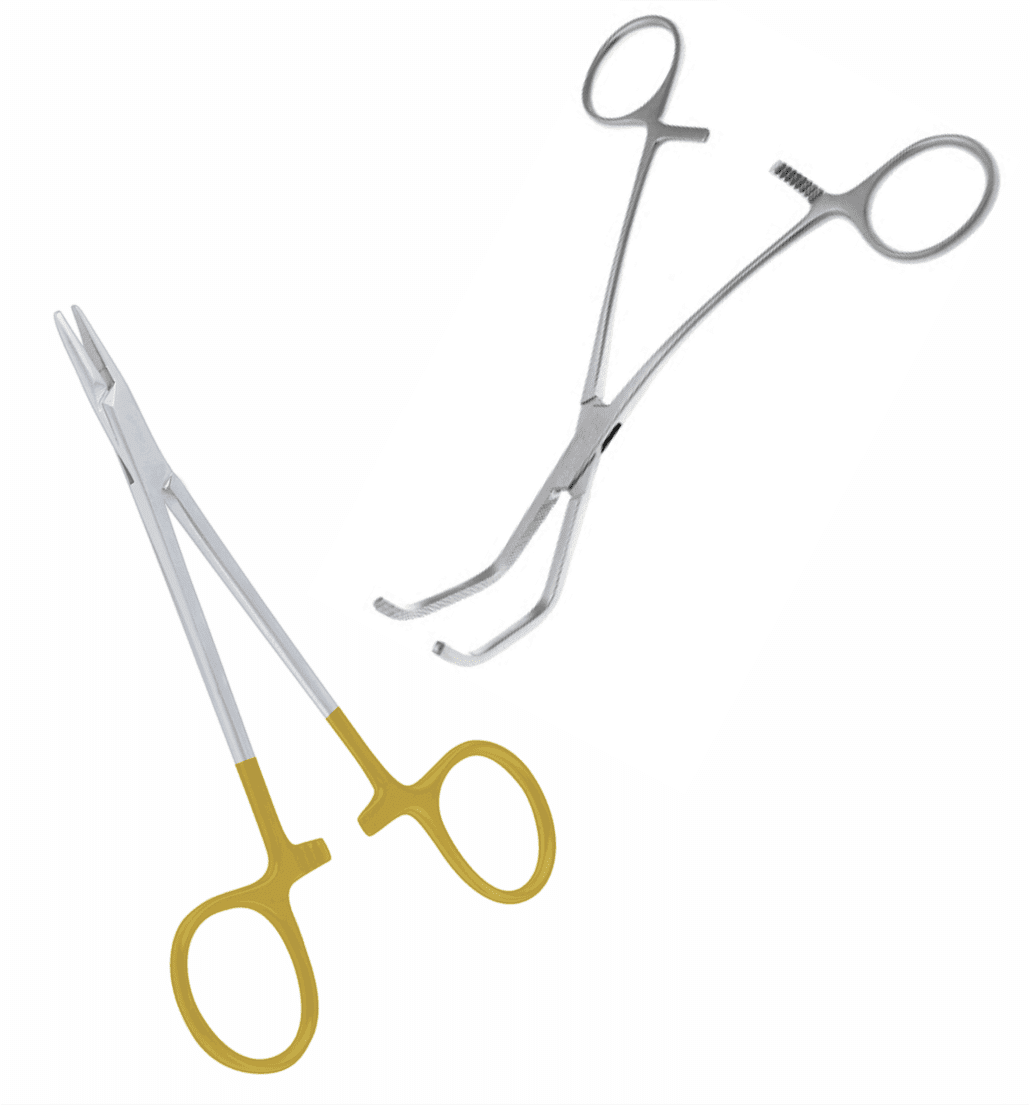
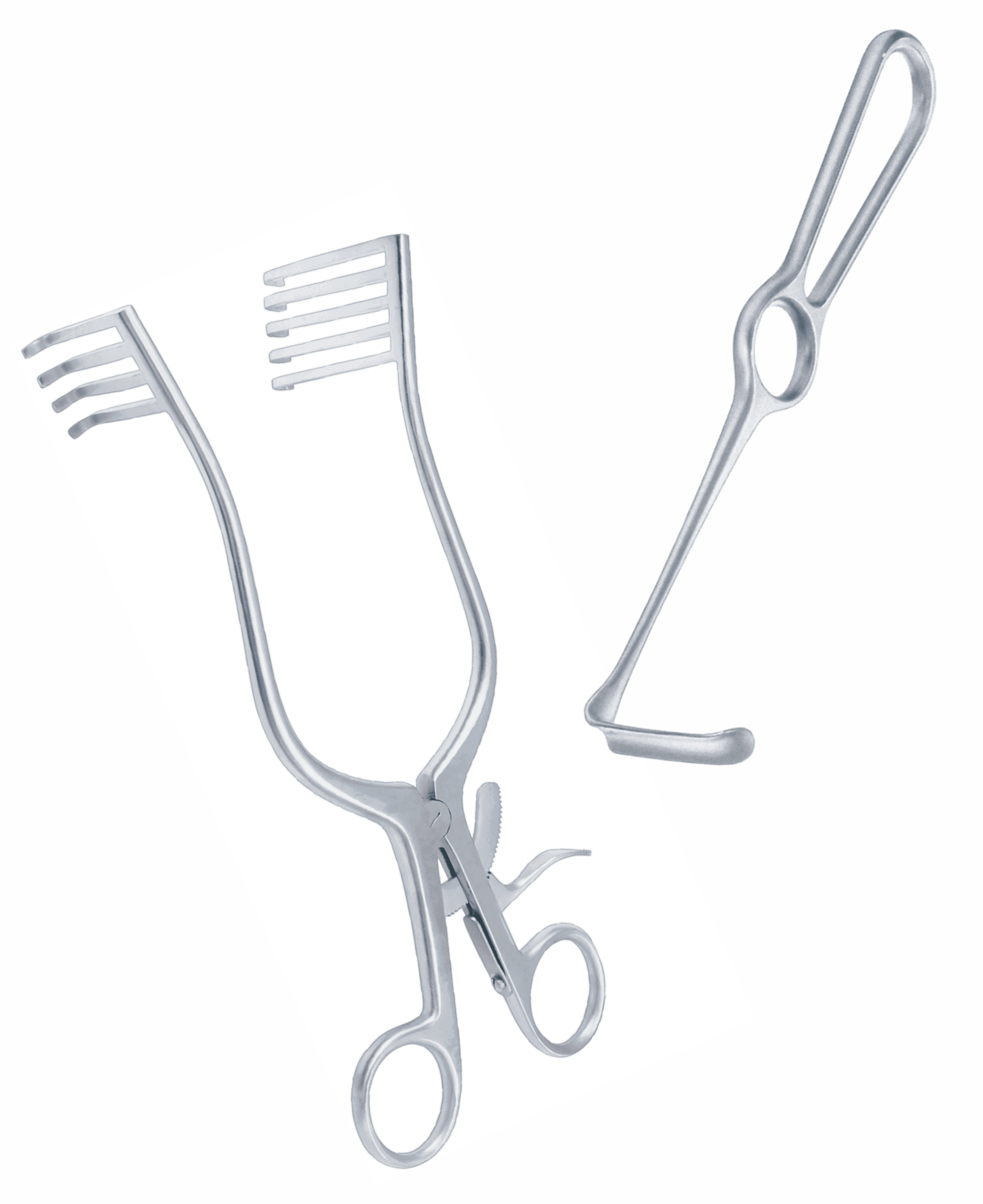
The variety, nomenclature and heritage of the surgical instrument marketplace is vast. It is so varied due to the complex range of procedures they feature in. Most instruments are named after their original inventor, the area of the body they are used and the type of device. For example, the Spencer Wells Artery Forceps was invented in the late 1800ʼs and is still one of the most common devices in use.
The Surgical instrument market value is estimated at more than £50m4. The challenge to retain the value and performance of devices, and the appropriate educational focus for NHS staff, is immense.
A case study presented on behalf of the ABHI SIG looked at 48 UK hospital sites of varying sizes in the UK (see page 9). An average hospital has 735 beds, 18 theatres and carries out 27,000 operations per year with an average of 1,545 surgical instrument sets on site. A typical reusable instrument set contains 48 instruments, with an approximate value per instrument of £40.00. On average a hospital has 75,000 instruments, with a value of around £3.6m. The likely number of instruments in circulation in the NHS is conservatively estimated at 17 million.
Single-use instruments are used alongside reusable instruments. In the single-use market there are common surgical areas that favour single-use devices, depending on the delicacy of the devices, safety and ability to re-clean reusable ones e.g. suction tube where cleaning and decontamination maybe difficult. Where patient outcome and diagnosis rely on, for example, a sharp device, single-use may be the only viable option.
Surgical instruments are not commodity products, they support positive surgical outcomes and shorter hospital stays. Investment in good quality equipment, strong supporting education, and high quality maintenance are essential
The sector continues to evolve, with the introduction of single-use devices which are Class IIa risk level in most cases. The imminent transition to the Medical Device Regulation will up-classify reusable instruments to Class I reusable, requiring notified body approval for the first time. Reusable instruments account for the vast majority of instrumentation, but the need for single-use devices must also be recognised.
With this up-classification, the obligation and cost for the manufacture of these devices goes up, in association with the recognition that their risk has increased. To navigate the challenges of Brexit and its interplay with the Medical Devices Regulation, the SIG has utilised its network to ensure such factors have been raised with appropriate stakeholders, particularly where it was felt these regulations could impact patient safety.
Understanding the cost and benefits of compliance with the new regulations should also be central to procurement decisions.
WHAT WE DO
THE VALUE OF WORKING WITH THE GROUP
Surgical instruments are essential for the delivery of modern healthcare. Their use is so widespread that they are easily taken for granted, and often little attention is paid to the origin, design, materials and decontamination protocols, or the regulatory processes and associated costs that are required for their introduction.
The supplier base for instruments is diverse, sourced from small family owned businesses, through to large multinational corporations. What they have in common are complex manufacturing processes, global supply chains, broad product ranges to suit varying clinical needs and product development with the capacity to innovate and change to meet clinical requirements. By joining ABHI, members show a commitment to transparent and ethical codes of manufacturing and business conduct, raising standards of quality and professionalism, and working to meet regulatory, technical and data requirements.
In order to be placed on NHS Supply Chain frameworks, manufacturers employ standards, whether national or international, to demonstrate compliance to the regulations which are audited by notified bodies. Separately, a manufacturer will also be audited to the ethical performance matrixʼ specified in the Labour Standards Assurance System (LSAS) and adhere to the requirements of the Modern Slavery Act 2015.
Labour Standards issues have been identified within this supply chain and the SIG have worked closely with NHS Supply Chain during the introduction of the LSAS to try to address these matters through the Surgical Instruments Frameworks. Reports have shown that progress has been made, although there is more work to be done in this regard.
The Modern Slavery assessment tool will be implemented imminently in this sector and ABHI members are committed to working with stakeholders to support ethical manufacturing and supply in this sector.
ABHI members support and co-operate with the NHS and Department for Health and Social Care initiatives in other initiatives such as, Scan4Safety, Sales Person Credentialing, and National Contracting.
Value based procurement5, a very recent initiative, enables NHS buyers to find the balance between cost, quality, support and ethical supply. The SlG recently produced the ‘Surgical Instrument Purchase and Care Guideʼ, provides guidance for purchasing and caring for surgical instruments. It can be downloaded from www.abhi.org.uk.
THE SAFETY OF SURGICAL INSTRUMENTS
Surgical instruments are important assets to any surgical unit or operating theatre. Instrument quality is key to the smooth running of operating theatres and ensuring patient safety.
SIG members provide collective user support and resources on the manufacture and safe use of both reusable and single-use surgical instruments. Individual member companies may also be able to provide guidance on more specialised surgical instruments.
What good looks like
- Design – Manufacturers take into consideration the instrument use and how it can be cleaned /decontaminated
- Regulation – Health Technical Memorandum (HTM) guide to be followed with all acceptance of instruments and their processing.
- Manufacture – Grade of steels need to be appropriate to allow correct function of instrument
- Correct Use – Instruction for use (IFU) from manufacturers should be followed e.g. Needle holders should not be used to remove screws or wires
- Procurement – Purchasing decisions must recognise the full value of products, not simply the acquisition price Quality, Safety and Value: The role of Surgical Instruments
- Reprocessing – Manufacturersʼ guidelines should be followed and IFUs should be relevant to the part of UK they are sold into. Note: HTMs are different for Wales & Scotland.
- Labelling/marking – All instruments need the appropriate CE mark. If single-use, it should be labelled with the correct symbol. Marking on instruments should be durable and does not deteriorate in the washing process.
- Maintenance – Maintenance programmes should be instigated to keep instruments in good condition e.g. sharpening service for scissors on a rolling programme.
If you delay an operation that’s an emergency, or have to use another set of instruments to achieve the same outcome – for example, where the surgeon has to change the procedure he/she planned to do because the correct instruments weren’t available – that’s putting patient safety at risk.”
The AFPP
“A surgeon had to change the procedure he was carrying out twice because of lost or broken instruments. Nobody can follow the order of the operating list. It is dictated by which instruments are available.”
Theatre Nurse
CASE STUDY – QUALITY OF REUSABLE INSTRUMENTS
A recent survey was conducted on typical hospital trusts. The information garnered showed that 70% of the sets listed contain handheld surgical instruments; the 7 rest is made up of telescopes and specific instruments for specialist procedures such as Orthopaedic and Neurosurgery. Additionally, there is another category called ‘supplementary instrumentsʼ which are the single packed and used when needed
All of these sets are used multiple times, some more than others, for example general, Dilatation and Curettage, delivery, tonsils.
The sets can contain anything up to 100 instruments which have to be processed each time they are used.
The data extracted from these audits can be utilised to investigate opportunities and the type of information to educate staff in theatres on what to look for and potential negative outcomes of not taking action. Similarly, as an MOT states roadworthiness for a motor vehicle, an instrument audit can clearly denote what is and what is not acceptable for use on a human being.
In summary, 65 audits were carried out in 48 hospitals over a 2 ½ year period. 32,000 instruments were checked.
The results were as follows:
- 31% needed replacement
- 33% needed repair
- 18% had issues with surface finish such as corrosion, water marks or presence of silicates
- 18% were acceptable.
There is a clear need for immediate investment in surgical instrument inventory. Instruments that are in need of repair or replacement pose potential an immediate patient risk if not picked up, and other issues such as surface finish can contribute to sterility issues.
It may well be that key areas of instrumentation are now more suited to single-use, particularly for those that may need regular repair or that are deemed not acceptable for surgical use.
In reference to the earlier market figures, to replace all of the instruments in need of repair would be an estimated cost of over £400m.
These issues need to be escalated to the relevant authorities to ensure that instruments used on patients are fit for purpose and not going to potentially cause more damage.
This document has been produced by members of the ABHI Surgical Instruments
Special Interest Section.
Association of British Healthcare Industries
107 Grayʼs Inn Rd, London WC1X 8TZ
www.abhi.org.uk